Presidential Address charts the long, winding road to engineering T cells
//
Estimated Read Time:
Engineering T cells is an elegant approach to treating cancer. But learning how to make T cells work in patients, selecting and engineering T cells to express cancer-antigen specific T cell receptors (TCRs) is not a straightforward process.
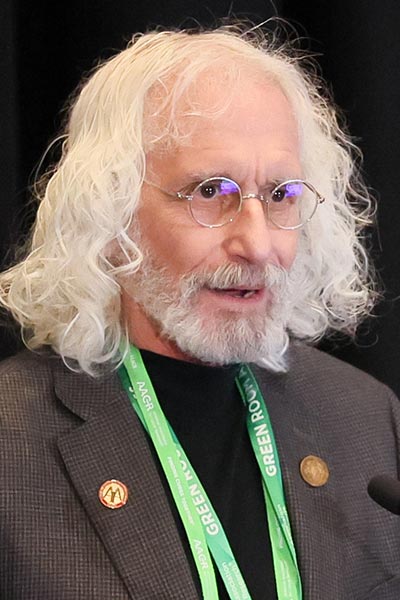
“There are a lot of steps and obstacles that are on the path to success and that need to be addressed,” said American Association for Cancer Research Immediate Past President Philip D. Greenberg, MD, FAACR, professor and head of immunology and the Rona Jaffe Foundation Endowed Chair, Fred Hutchinson Cancer Center. “This is about disabling or rewiring immunosuppressive mechanisms operative in the TME (tumor microenvironment) by engineering the T cells and also overcoming T-cell death and exhaustion due to chronic stimulation.”
Greenberg explored his own continuing experience engineering T cells during the Presidential Address: Engineering T Cells to Eradicate Tumors – Identifying and Overcoming the Obstacles on Sunday, April 7, at the AACR Annual Meeting 2024. The session is available on demand for registered Annual Meeting attendees through July 10, 2024, on the virtual meeting platform.
Engineering T-cell therapy begins with target selection, but tumor evasion from antigen loss may limit efficacy. Another key step is to select an appropriate TCR with high affinity and high avidity that exhibits no alloreactivity or cross-reactivity with normal self-proteins. And while immune suppression, cell death, and T-cell exhaustion are common obstacles, synthetic biology can be used to maintain T-cell function.
TCRs are typically engineered to respond to one of three broad classes of tumor antigens: over-expressed antigens, cancer testis antigens, and neoantigens. Regardless of the type of antigen, rapid, high-throughput isolation of high-affinity native TCRs that are specific for defined targets is essential, Greenberg noted. Manual isolation is too labor intensive to be practical.
His lab engineered CD8 T cells transduced with high-affinity WT1-specific TCR to prevent acute myeloid leukemia (AML) relapse after hematopoietic cell transplantation (HCT). WT1-specific T cells were highly effective in preventing relapse post-HCT, but not for treating relapsed and/or progressing AML.
“We asked, can we interrogate that treatment arm to learn about what were the immune evasion obstacles that were interfering with our ability to get better responses in that subset of patients?” Greenberg said.
Researchers found multiple problems and potential solutions. The targeted WT1 epitope required processing by the immunoproteasome (IP) and some patients lost the required IP expression. So researchers identified a different epitope that is more robustly processed and presented.
Reduced expression of the epitope could result from epigenetic modification of the gene encoding the antigen. The researchers explored whether epigenetic modification can be targeted.
T cells can become dysfunctional or exhausted. Synthetic molecules can be engineered to help sustain T-cell function and resist cell death, Greenberg noted.
CD8 T cells have poor persistence or undergo cell death due to lack of assistance to counteract persistent stimulation and toxicity, he explained. To overcome this, T cells can be engineered to resist cell death. It is also possible to build a TCR with coordinated CD4 and CD8 response to support sustained immunity and anti-tumor activity.
Many of the lessons learned from engineering T cells to treat AML can also be applied to solid tumors, Greenberg said. T cells engineered with mesothelin-specific TCRs lyse human pancreatic ductal adenocarcinoma cells in mice, he noted, but the effect is transient.
Further work showed that T cells persisting at the tumor site progressively upregulate inhibitory receptors and become dysfunctional. Repeated T cell infusions can sustain anti-tumor activity and prolong survival, forming the basis for an ongoing clinical trial.
T-cell therapy in general has two major problems, Greenberg continued, T-cell survival and T-cell dysfunction. Most transferred CD8 T cells do not persist or survive in the context of advanced or rapidly progressive disease. And CD8 T cells that do persist too often become dysfunctional due to inhibitory signals, metabolic stress, and suppressive cytokines. Synthetic immunomodulatory fusion proteins (IFPs) can convert inhibitory and death signals into co-stimulatory, proliferation, and survival signals.
In mice with pancreatic cancer, T cells that express Fas-41BB exhibit increased proliferation, decreased apoptosis, and increased metabolic fitness, leading to enhanced mouse survival.
CD4 T cells also help support CD8 T-cell function, proliferation, and survival, enhance direct and indirect killing of tumor cells, drive B-cell maturation and antibody production, and delay or prevent T-cell exhaustion.
Work is currently underway to engineer a composite interactive CD4/CD8 T-cell response with IFP co-stimulation to target KRAS. Another trial with T cells engineered to express both a KRAS-specific TCR and the Fas-41BB IFP recently opened for enrollment.
Ongoing research aims to rewire cytokine receptors, identify protein degradation targets, and explore other novel approaches to synthetic biology.
“It has been a very long and winding road to get to where we are,” Greenberg said. “We still know we have a way to go, and there will be more bends in the road, but to quote Jerry Garcia, ‘What a long, strange trip it’s been.’”




