Study findings highlight potential of novel immunotherapy strategies
//
Estimated Read Time:
While the introduction of immune checkpoint inhibitors revolutionized the oncology field, patients may develop resistance to these drugs and have limited options beyond these therapies. Fortunately, researchers are exploring immunotherapy approaches beyond immune checkpoint inhibitors, including novel CAR T cells, bispecific antibodies, and oncolytic viruses.
In the clinical trials plenary session Beyond Immune Checkpoint Inhibition: Novel Immunotherapy Strategies on Sunday, April 7, four experts discussed emerging results from clinical trials evaluating novel immunotherapies. This session was chaired by James L. Gulley, MD, PhD, clinical director of the National Cancer Institute, and Shivaani Kummar, MD, co-deputy director of the Oregon Health & Science University Knight Cancer Institute.
This session is available on demand for registered American Association for Cancer Research Annual Meeting 2024 participants through July 10, 2024, on the virtual meeting platform.
Linvoseltamab in patients with relapsed or refractory multiple myeloma (RRMM)
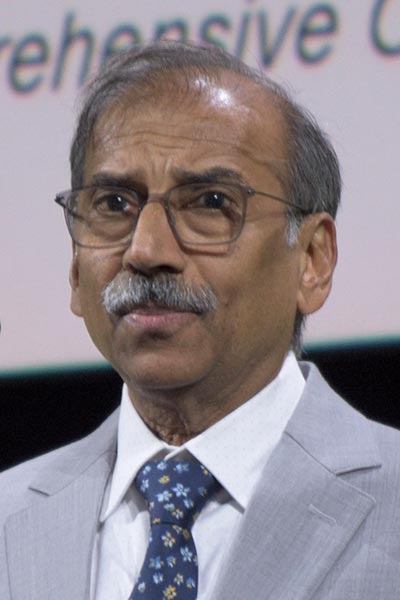
Sundar Jagannath, MD, director of the Multiple Myeloma Center of Excellence at the Tisch Cancer Institute at Mount Sinai Hospital, presented pivotal results from the LINKER-MM1 clinical trial. The LINKER-MM1 study tested the safety and efficacy of linvoseltamab, a B-cell maturation antigen (BCMA)-targeted, T-cell engaging bispecific antibody, for the treatment of RRMM.
“Bispecifics are a very effective, off-the-shelf treatment option for patients with heavily pretreated multiple myeloma,” Jagannath said. “The overall response rate for currently approved BCMAxCD3 bispecific antibodies range between 61 and 63 percent.”
Linvoseltamab induced high rates of deep and durable responses in patients with late-stage RRMM, most of whom were refractory to at least three prior lines of treatment, including those in prespecified high-risk groups. Linvoseltamab had an acceptable safety profile; the most common treatment-emergent adverse events were cytokine release syndrome (CRS), neutropenia, and anemia. Importantly, the incidence of most adverse events decreased over time.
CTX130 in patients with advanced clear cell renal cell carcinoma (ccRCC)

Samer A. Srour, MB ChB, MS, assistant professor at the University of Texas MD Anderson Cancer Center, presented long-term follow-up data from the COBALT-RCC study. The COBALT-RCC study was a phase I dose-escalation study of CTX130, a CD70-targeting allogeneic CAR T-cell therapy, in patients with ccRCC.
Thirty percent of ccRCC patients have metastatic disease. The current standard of care therapy for these patients is either a combination of two immune checkpoint inhibitors or a checkpoint inhibitor with vascular endothelial growth factor (VEGF)-directed therapy. “When you fail these standard treatments, those patients have an overall poor prognosis,” Srour said.
CTX130 produced a durable complete response in one patient, which remains ongoing after three years, a noteworthy outcome for allogeneic CAR T-cell therapy, Srour said. Further, CTX130 had an acceptable safety profile with no graft versus host disease or immune effector cell-associated neurotoxicity syndrome. Based on these promising results, researchers have made additional edits to CTX130 to enhance its potency and persistence. The result, CTX131, is now being tested in clinical trials.
RP1 in solid organ transplant (SOT) recipients with advanced cutaneous malignancies

Michael R. Migden, MD, professor at the University of Texas MD Anderson Cancer Center, presented initial results from the ARTACUS clinical trial.
“Non-melanoma skin cancer is the most common post-transplant malignancy in SOT recipients and occurs at a seven- to 53-times higher incidence versus the general population,” Migden said. He explained that immune checkpoint blockade is not recommended for patients with SOT-associated non-melanoma skin cancer due to the risk of transplant rejection.
However, the oncolytic immunotherapy RP1, in combination with intravenous nivolumab, demonstrated deep and durable responses in non-SOT patients with advanced skin cancers. The ARTACUS trial is an open-label, phase Ib/II study assessing the safety and efficacy of RP1 in SOT recipients with non-melanoma skin cancer.
RP1 showed robust antitumor activity, and most responses are ongoing. Further, RP1 was well tolerated, with a safety profile similar to that of non-immunocompromised patients with advanced skin cancers. The most common treatment-emergent adverse events were fatigue, chills, and pyrexia. Importantly, no allograft rejection was observed.
Talimogene laherparepvec (TVEC) in patients with invasive cutaneous squamous cell carcinoma (cSCC)

Clara N. Curiel-Lewandrowski, MD, professor of medicine at the University of Arizona, presented results from a single-arm, phase II study of TVEC in patients with invasive cSCC.
“The challenging landscape of cSCC is highlighted by three main components: … the increased incidence of cSCC that we are observing across multiple populations, the multiplicity of primary tumors within a single individual, and the decreased survival associated with these diagnoses,” Curiel-Lewandrowski said.
TVEC is a herpes simplex virus type 1 oncolytic immunological agent approved by the FDA for the local treatment of unresectable melanoma. In patients with low- or intermediate-risk cSCC, intralesional injection of TVEC demonstrated a rapid and robust overall response, with responses observed in all injected tumors. Further, TVEC may decrease the rate of new primary cSCC tumors and may induce an abscopal effect on neighboring lesions. Treatment with TVEC was generally well tolerated, with mostly mild and transient adverse events.




